Sport Psychology During a Tournament
14 March 2024
Osteoarthritis- the latest treatment options: Physiotherapy and more!
25 July 2024Dedicated to all the wonderful teammates, coaches, and rivals.
Written by: Arjun Patel, PT, MPT, MCPA, Clinic Director: Blue Space Clinic Physiotherapy
Please note that post/document is for information purposes only. If you have any questions or need medical advice please see a healthcare professional.
Go the the relevant section based on your symptoms:
1. Dull/ sharp pain, or general soreness: Orthopedic Injuries
Examples of Orthopedic Injuries
The P.E.A.C.E. and L.O.V.E. Protocol in case of an injury
Who to see
Do I need imaging?
Signs and Symptoms (NOT LIMITED TO THIS LIST)
Role of Immediate Action
Who to see
Do I need imaging?
Numbness, tingling, pins and needles, and burning- Neuro Injuries
Who to see
Do I need Imaging?
Dull/ sharp pain, or general soreness: Orthopedic Injuries
Orthopedic injuries encompass a range of conditions that can affect athletes during training or competition. From ankle sprains to knee ligament tears, fractures, and even DOMS (Delayed Onset Muscle Soreness), it’s essential for athletes to be aware of these injuries and their management.
Examples of Orthopedic Injuries
Sprains:
Sprains occur when the ligaments supporting a joint (knee, ankle, wrist) are stretched or torn, often due to a sudden twist or turn, or due to contact. Symptoms include pain, swelling, and difficulty bearing weight. To manage this, follow the P.E.A.C.E. and L.O.V.E. protocol and read the information below.
Strains:
Strains occur when a muscle is torn. There are different degrees of tear, with most strains being minor. Symptoms can include pain, swelling, and difficulty with moving that particular muscle. In severe cases you can have bruising. To manage this, follow the P.E.A.C.E. and L.O.V.E. protocol and read the information below.
Fractures and other serious injuries :
Fractures, or broken bones, can occur in various parts of the body due to trauma or overuse. Common sites for fractures in athletes include the wrist, ankle, and bones of the lower leg, but also stress fractures in smaller joints. This is always a medical emergency. Call 911 and go to the emergency department right away.
DOMS (Delayed Onset Muscle Soreness):
DOMS refers to muscle soreness and stiffness that develops 24 to 48 hours after strenuous exercise. While not a serious injury, DOMS can significantly impact athletic performance and comfort.
P E A C E and L O V E- Protocol in case of an injury:
- P.E.A.C.E. Protocol (Protection, Elevation, Avoid Anti-inflammatory modalities, Compression, Education):
- Protection: Protect the injured area from further harm by using supportive equipment, such as braces or crutches, if necessary.
- Elevation: Elevate the injured limb above the level of the heart to reduce swelling and promote circulation.
- Avoid Anti-inflammatory Modalities: Contrary to traditional approaches, avoid using anti-inflammatory medications during the initial stages of injury, as they may interfere with the body’s natural healing processes.
- Compression: Apply gentle compression to the injured area using bandages or compression garments to minimize swelling and provide support.
- Education: Educate yourself about your injury, its management, and the importance of following a structured physical therapy program.
- L.O.V.E. Protocol (Load, Optimism, Vascularization, Exercise):
- Load: Gradually introduce appropriate loading to the injured area as tolerated, focusing on restoring function and strength while minimizing pain.
- Optimism: Maintain a positive outlook throughout the physiotherapy process, recognizing that setbacks may occur but progress is possible with dedication and patience.
- Vascularization: Promote blood flow to the injured area through gentle movement to facilitate healing and reduce stiffness.
- Exercise: Engage in targeted rehabilitation exercises prescribed by a healthcare professional to improve range of motion, strength, and proprioception, ultimately facilitating a safe return to sport.
Pharmacological Management
- Pharmacological management may involve pain relief medications, such as acetaminophen, ibuprofen, or naproxen to manage discomfort during the acute phase of injury. However, it’s essential to consult with a healthcare professional before starting any medication regimen.
Who to see
Minor orthopedic injuries resolve on their own in approximately a week. For anything lasting more than that, please see your healthcare provider (GP or Physiotherapist.).
Do I need imaging?
Gold standard for diagnosing most orthopedic injuries is a combination of physical exam, and imaging such as ultrasound, x-rays, or MRI. Depending on your injury, your healthcare provider will consult and refer you for imaging if needed.
Head Injuries- Concussions
As per law, suspected concussions and head injuries should enter a removal from play protocol in Ontario. Concussions vary in presentation and recovery from person to person.
Signs and Symptoms (NOT LIMITED TO THIS LIST):
- Headache or pressure in the head
- Dizziness or balance problems
- Nausea or vomiting
- Confusion or feeling mentally foggy
- Sensitivity to light or noise
- Changes in mood or behavior
- Loss of consciousness
Role of Immediate Action:
Stop and Monitor: No two concussions are alike. Even if you had a concussion before, your symptoms this time may be different. If you suspect a concussion, it’s vital to immediately cease activity and monitor your symptoms closely. Continuing to play can exacerbate the injury and hinder recovery.
Removal from Play for 30 Days: Recognizing the individuality of concussions, athletes suspected with this injury should go to EMRG, should be removed from play for a minimum of 30 days or until symptom-free and cleared by a healthcare provider trained in concussion management.
Who to see
Acute symptoms: Go to emergency to rule out other injuries and red flags
Afterward: if you have a concussion diagnosis, see a Physiotherapist specializing in concussion rehabilitation. Further referrals for neuropsychology or a physiatrist may be necessary depending on your symptoms duration. See our blog on concussions for further details.
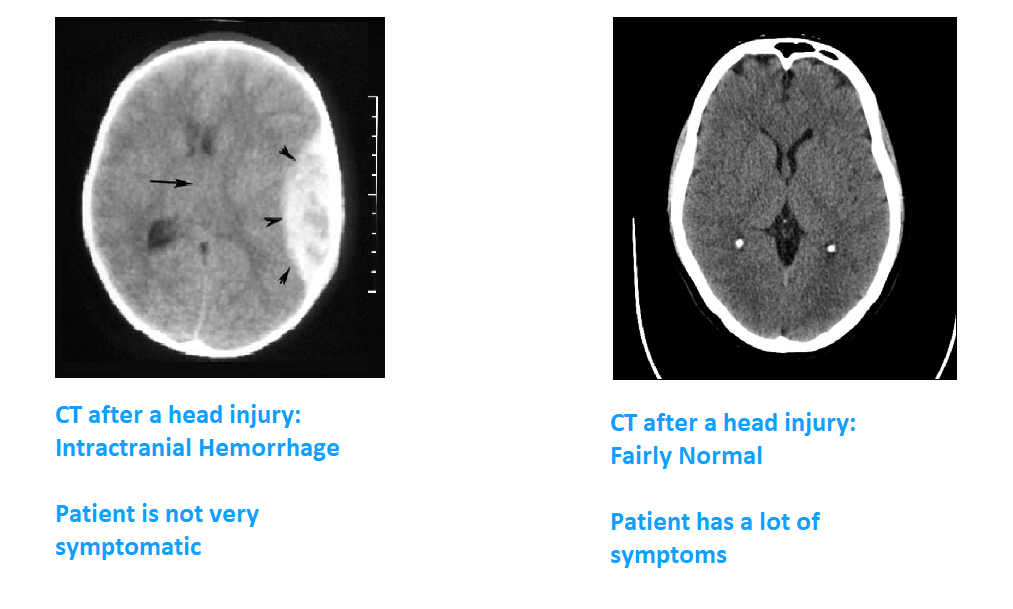
Do I need imaging?
Concussions can’t be diagnosed by imaging; however, other, more serious injuries, such as intracranial hemorrhage, or other brain injuries can be ruled out using CT scans for example.
Numbness, tingling, pins and needles, and burning- Neurological Injuries
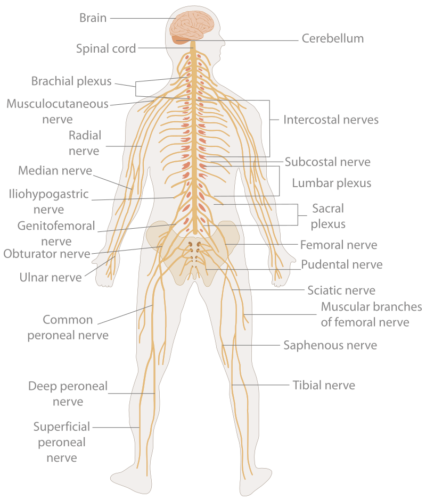
Neurological injuries can occur after usually pulling or stretching traumatic injuries, or secondary to other injuries during athletics.
These are often characterized by temporary weakness, numbness, tingling, pins and needles, and burning sensations in the affected area. Neuro injuries can be serious if unchecked.
Immediate Response: If you experience any of the above symptoms during training or competition, stop and assess the situation. Continuing to push through could exacerbate the injury.
Who to see
For mild injuries and symptoms, you can see your family doctor or physiotherapist.
If you are having major symptoms such as a loss of a limb function or weakness that is not going away, or a lot of tingling/ numbness etc., go to emergency right away. Once the acute phase of the injury has passed, rehabilitation is needed to return the affected limb to normal and return to full function. Physical therapy plays a crucial role in restoring function and preventing future injuries.
Do I need Imaging?
X-rays, MRIs (Magnetic Resonance Imaging), or CT scans (Computed Tomography) may be ordered to visualize the affected area and assess for any structural damage or abnormalities that may be impacting the nerves. Nerve conduction studies may be needed in severe injuries or complex cases to evaluate the function of nerves and muscles and can help identify any underlying nerve damage or dysfunction.